Oxygen keeps the body running, powering every cell from the brain to the muscles. But it doesn’t just float through the bloodstream on its own — instead, it relies on red blood cells to get where it needs to go. These cells are specialized couriers, delivering oxygen from the lungs to the tissues that need it most.
Recent research into cell metabolism and immune function has highlighted potential new players in red blood cell health, including the C15 fatty acid, which has been studied for its role in cellular resilience. Learning how red blood cells transport oxygen is key to understanding energy, focus, and overall health.
What Do Red Blood Cells Do?
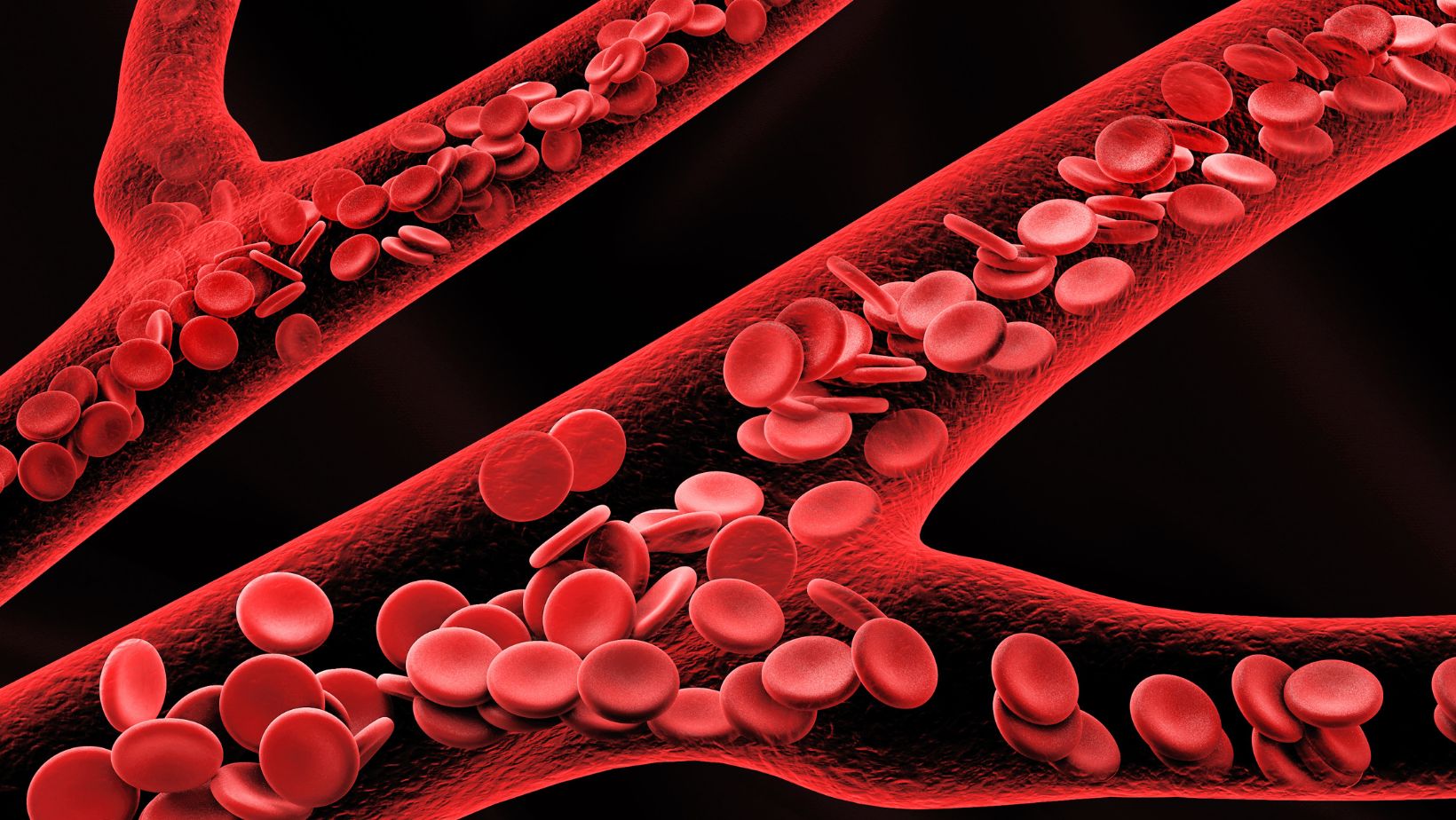
Red blood cells, or erythrocytes, are responsible for transporting oxygen throughout the body. They do this with the help of a protein called hemoglobin, which binds to oxygen molecules in the lungs and carries them through the bloodstream. Once red blood cells reach tissues with lower oxygen levels, hemoglobin releases the oxygen to be used for energy production.
These disc-shaped cells lack a nucleus, which gives them more room to carry hemoglobin. This distinct shape also helps them squeeze through tiny capillaries and maximize surface area for gas exchange.
Red blood cells are produced in the bone marrow and regulated by a hormone called erythropoietin, which the kidneys release in response to low oxygen levels. On average, red blood cells live about 120 days before being broken down and replaced by new ones.
How Do Red Blood Cells Carry Oxygen?
Oxygen transport starts in the lungs, where red blood cells pick up oxygen that’s been inhaled. Each hemoglobin molecule can bind up to four oxygen molecules. This binding is reversible and highly responsive to changes in oxygen concentration.
In areas where oxygen is abundant, such as the lungs, hemoglobin binds tightly to it. In areas where oxygen is scarce, like active muscles, hemoglobin releases it so cells can use it for energy.
Oxygen is carried in two main ways. Most oxygen is bound to hemoglobin, while a small amount dissolves directly into blood plasma. The efficiency of oxygen delivery is often measured using oxygen saturation levels, which reflect the percentage of hemoglobin molecules carrying oxygen.
Clinicians use tools like pulse oximeters to monitor this metric, especially in critical care or respiratory conditions. Effective oxygen transport is essential for maintaining organ function, physical performance, and mental clarity.
What Factors Influence Oxygen Delivery?
Oxygen delivery isn’t just about how much is in the air or how many red blood cells are present. Rather, it’s affected by the conditions inside the body.
One major factor is pH. When blood becomes more acidic — which can happen during intense exercise or illness — hemoglobin releases oxygen more readily. This is known as the Bohr effect. Similarly, higher levels of carbon dioxide or elevated body temperature can also prompt hemoglobin to unload more oxygen into tissues.
Another key player is a molecule called 2,3-Bisphosphoglycerate (2,3-BPG), which is produced by red blood cells. It helps fine-tune hemoglobin’s oxygen-releasing behavior, especially under conditions like high altitudes or chronic lung disease. When levels of 2,3-BPG increase, hemoglobin holds onto oxygen less tightly, improving delivery to where it’s needed.
All of these variables help the body adapt in real time, ensuring that oxygen goes where it’s needed most under changing conditions.
What Happens When Red Blood Cell Function Is Impaired?
When red blood cells can’t do their job, oxygen delivery suffers, and the effects are noticeable. In conditions like iron deficiency anemia, there isn’t enough hemoglobin to carry sufficient oxygen. As a result, people often feel fatigued, dizzy, or short of breath.
Sickle cell disease is another example, where red blood cells take on a rigid, sickle-like shape that makes it harder for them to move through blood vessels and deliver oxygen effectively. These misshapen cells also have a shorter lifespan, leading to chronic anemia.
Carbon monoxide poisoning can block oxygen transport altogether. Hemoglobin binds to carbon monoxide more strongly than it does to oxygen, leaving the body starved of the oxygen it needs, even if breathing appears normal.
These examples highlight how sensitive the human body is to disruptions in oxygen transport. Even small changes in red blood cell function can have major impacts on health and performance.
Why Oxygen and Red Blood Cells Matter
Red blood cells are crucial to keeping your body energized, focused, and functioning. By efficiently transporting oxygen, they support everything from muscle movement to brain activity. When their function is disrupted, the effects are immediate and wide-reaching.
While often overlooked, red blood cell health is foundational to overall wellness. Understanding how oxygen is carried and delivered can help inform smarter health choices and highlight the importance of supporting these tiny cells.



